Improved efficiency and reduction in plan variation were two of the reasons Colin Hornby, radiotherapy advisor to the Health and Wellbeing Division of the Department of Health and Human Services in Melbourne, Australia (a state government agency) proposed a statewide collaborative in Victoria.
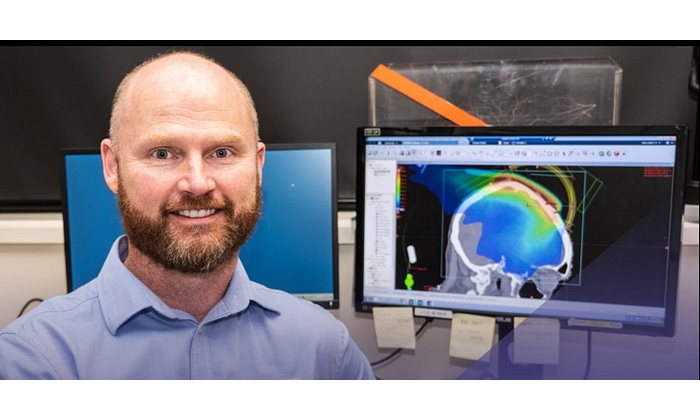
 Colin Hornby, radiotherapy advisor for the Victoria Department of Health and Human Services
Colin Hornby, radiotherapy advisor for the Victoria Department of Health and Human Services
As a result of that proposal, government-funded radiation oncology clinics in the state of Victoria began a statewide implementation of Varian’s RapidPlan™ knowledge-based treatment planning software and began providing each other with mutual support, sharing techniques and models. The goal was to improve the quality of radiotherapy treatment by using RapidPlan to predict treatment and plan outcomes and then use these predictions to optimize IMRT plan parameters, according to Hornby.
“RapidPlan was a game-changer,” says Hornby, who has been dosimetrist for 40 years. “You don’t see such potential for significant improvement every day, so I proposed the state government purchase RapidPlan licenses for eight Eclipse™ systems being used at public treatment sites across Victoria. From there, we started building models in RapidPlan and using them at every Eclipse site (now nine) to help reduce the many variables inpatient care across rural and metropolitan areas.”
In a recently published joint paper, Hornby and collaborators from across Victoria describe the development of this multicenter model in planning prostate treatment.* The consortium also has been able to build models out of shared data pools—about 10,000 treatment courses combined—expanding from prostate to head and neck, brain, anus, and rectum. Anal cancer is not that common, Hornby says, but with cases pooled from several sites, the model is relevant and turned days of planning into a few hours. It’s also being used by some sites as a model for gynecological cancer treatment planning.
“Since RapidPlan uses machine learning to extract knowledge, it’s made it possible for a lot of people to get together and share their expertise,” Hornby says. “Now those sites are collaborating, they’re also thinking more broadly about radiation oncology and aligning other efforts.”
Barwon Health’s Andrew Love Cancer Center, Geelong, Australia
Phillip Moloney is a radiation therapist at Barwon Health’s Andrew Love Cancer Center in Geelong, a rural area of Victoria about 50 miles from Melbourne. The center, which treats about 85 patients a month, is part of the statewide collaborative cooperating to improve the quality of radiotherapy treatment by using RapidPlan knowledge-based treatment planning.
 Phillip Moloney, radiation therapist at Barwon Health’s Andrew Love Cancer Center
Phillip Moloney, radiation therapist at Barwon Health’s Andrew Love Cancer Center
“RapidPlan immediately sped up our planning process and improved the consistency of plan quality,” Moloney says. “Not only did we save contouring time, but the junior dosimetrists typically got to the optimal plan after just one run-through, even without previous experience of a particular scenario.”
Moloney also notes that over time, the plan quality has improved and as models are updated, machine learning in RapidPlan helps the clinic create even better plans.
“It’s reassuring to use a RapidPlan model and know that we’re using similar plans to the US or Europe, even if it’s something that we may only see once or twice a year,” he says. “It gives us the confidence that we’re meeting the standard of a world-renown cancer center.”
Discover more about the machine learning features in RapidPlan knowledge-based planning.
_________________________________________________
*Panettieri V. et al. (2019), Development of a multicentre automated model to reduce planning variability in radiotherapy of prostate cancer. Physics and Imaging in Radiation Oncology, 11 , pp. 34-40.
The information captured herein represents the genuine experience of the attributed individuals and may not necessarily represent the views of Varian or the above-referenced institution. Individuals were not compensated for their participation. Radiation treatment may not be appropriate for all cancers. Individual results may vary.